By Nicole Ireland
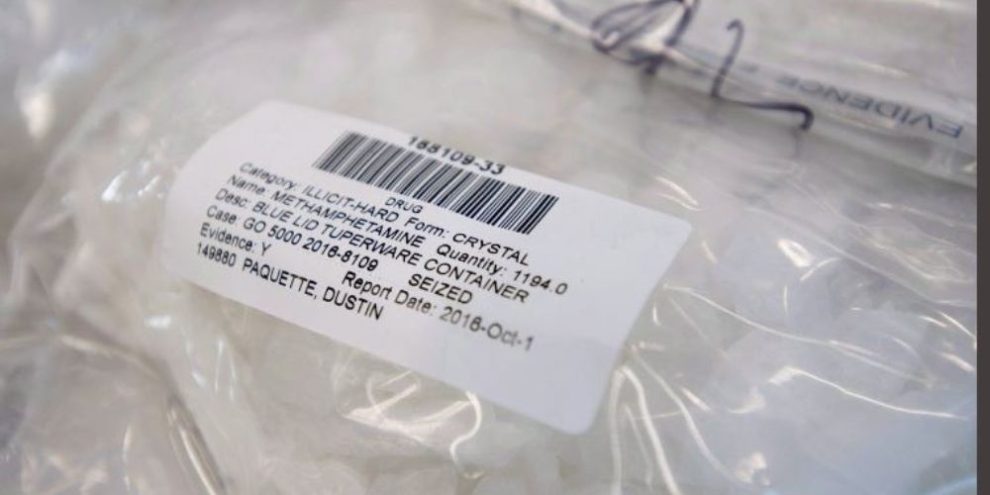
Amphetamine-related visits to Ontario emergency departments have skyrocketed over the last two decades, a recent study published in the Canadian Journal of Psychiatry says.
"It's astonishing,” said lead author James Crispo, a postdoctoral research fellow in pharmaceutical sciences at the University of British Columbia who is based in Sudbury, Ont.
The researchers used health administrative data to review adult emergency department visits throughout Ontario between January 2003 and December 2020.
They found that the number of ER patients suffering from an amphetamine-related condition increased almost 15 times over that time period.
Because they eliminated prescription amphetamines, which are sometimes used to treat ADHD, researchers believe the majority of the emergency department visits were specifically due to methamphetamine, or meth — a stimulant street drug that has become increasingly prevalent in Canada.
The study showed an especially sharp increase between 2015 and 2020.
Emergency departments in Western Canada and the Prairies have also seen dramatic increases in patients arriving with meth-related illness, said Sarah Konefal, senior research and policy analyst with the Canadian Centre on Substance Use and Addiction.
There has also been an "uptick" in Quebec, she said.
The Atlantic provinces have not seen the same rise in meth use, Konefal said, as cocaine is "by far much more prominent" in that region.
Dr. Arun Abbi, an emergency physician at Foothills Medical Centre and the Peter Lougheed Centre in Calgary, said they started seeing an influx of patients who had taken meth well before Ontario hospitals did.
Patients are "agitated" and are often brought to the emergency department by police "because they're hallucinating and paranoid, sometimes yelling," Abbi said.
Meth-induced psychosis is a huge problem, he said.
“When you look at our psychiatric ward, often 50 per cent of the people admitted to short stay are meth-induced psychosis," he said.
"It often affects our flow for mental health patients because we're often holding a lot of mental health patients in Emerg because there's no inpatient capacity."
Many people who use methamphetamine are marginalized, Konefal said.
People who are homeless, for example, may use meth "to stay awake (to) guard their belongings," she said.
Abbi said that's consistent with what he sees in practice. He estimates the vast majority of patients who come to the hospital due to meth are homeless.
Another significant issue across the country is that people often use more than one drug, mixing a stimulant — like meth or cocaine — with an opioid, such as fentanyl, said Konefal.
That can either be intentional or unintentional, she said, and can lead to overdoses. People may not realize the meth or cocaine they're taking are laced with fentanyl. Or, they may mistakenly believe that taking a stimulant drug will counteract an opioid overdose.
In fact, "combining opioids and stimulants can generally make it more likely that someone might experience an overdose because one masks the other," she said, leading someone to take too much opioid as they're not feeling the effects.
The Ontario emergency department study found that about one-third of the people on amphetamines also use opioids, Crispo said.
"This is very much an issue of polysubstance use," he said.
"Whether it's opioids or whether it's amphetamines, I think we have a problem. And this problem needs critical investment."
Part of that investment needs to be directed toward research on how to treat methamphetamine use disorders, Crispo said.
While medications, including methadone and suboxone, are available to ease the withdrawal symptoms of opioid addiction, there's no such long-term treatment to help patients manage meth cravings, Abbi said.
Emergency physicians can only give short-term relief by sedating patients suffering from meth psychosis, then discharging them when they're stable, he said, noting that more residential treatment services — along with access to housing — are needed in the community.
One of the limitations of the Ontario emergency department study, Crispo said, was that if someone didn't have a health card, their data wasn't included in the study.
That means that some vulnerable or transient patients may not have been counted — and the increase in amphetamine-related emergency visits could be even bigger than the study suggests.
"It's probably an underestimate of what's actually going on,” Crispo said.
Banner image: THE CANADIAN PRESS/Jonathan Hayward
This report by The Canadian Press was first published March 15, 2023.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.